Although the phenomenon of decompression sickness (DCS) is not fully understood, there are widely agreed upon factors that contribute to one’s susceptibility to it. Anything that affects our circulatory system, i.e. increases/decreases/hinders blood flow, affects the rate of on-gassing and off-gassing. Therefore, anything that affects our circulatory system affects our risk of developing DCS.
In this installment of our Education series, we are going to take an in-depth look at exactly what makes a diver more likely to develop DCS. Continue reading to find out how to mitigate the risks.
Dehydration

Dehydration is considered to be one of the greatest factors affecting the risk of developing DCS. In most cases of DCS, the diver is found to be dehydrated. That being said, however, dehydration is also a consequence as well as a cause of DCS, so the evidence may be slightly skewed.
Although there is actually little clinical evidence proving the link between DCS and hydration, considering that water composes so much of our body and is vital for maintaining its proper function, it is unsurprising that it could play a key role in affecting our susceptibility to DCS.
The main theory is that when we are dehydrated there will be less plasma in the blood which will hinder gas transport, and therefore hinder off-gassing. Similarly, as bubbles form and duplicate, they make surrounding tissues more permeable, leading to more water from the circulatory system leaching into surrounding tissues. This results in dehydration. The latter problem demonstrates that dehydration is not only a cause of DCS, but is also a consequence too.
Many of us are in a state of continuous dehydration without realising, as we have become used to being in this deprived state and rely on other less hydrating or even dehydrating liquids, e.g. coffee, alcohol, fruit juices. Diuretics such as tea and coffee can result in dehydration. Similarly, alcohol, nausea, diarrhoea, flying, and sweating are also common contributors to dehydration.
Diving itself also poses the potential to dehydrate the diver. The breathing of very dry air causes rapid loss of liquid as your mouth and throat continually attempt to moisten the inspired air. Similarly, the gearing-up process combined with tropical environments also creates the perfect conditions for dehydration.
Luckily for us, dehydration is one of the easiest factors to control. The daily recommendation is a minimum of two litres of water per day, usually amounting to 8-10 glasses. However, in many cases, the body requires more liquid, especially when in warmer environments and/or when having engaged in physical exercise.
If you are a diver looking to improve your safety (which all divers should be!) then aiming to improve your hydration is key to risk mitigation.
Temperature

When skin temperature begins to drop, blood flow to the extremities is reduced. This is known as vasoconstriction and reduces overall heat loss. However, this will result in less blood flow.
Similarly, when skin temperature increases, blood flow to the extremities will increase in order to maintain a constant internal temperature and therefore prevent overheating. This is known as vasodilation. This will result in more blood flow.
In diving, maintaining a constant temperature is ideal, whether that is higher or lower than average temperature. The problem begins when body temperature changes throughout the dive. The reason for this is simple.
If we begin the dive warm, our cells will be vasodilated, meaning that on-gassing will be happening across the body at a normal rate. If we then become progressively colder during decompression, our cells will vasoconstrict, resulting in less blood flow, and therefore a slower rate of off-gassing.
The problem is that our dive computer/decompression algorithm does not account for this reduction in the rate of off-gassing as it cannot measure the temperature of our body. Therefore, we will end the dive with a higher amount of dissolved inert gas than our computer assumes us to have. Obviously, in marginal cases, this increases the risk of DCS.
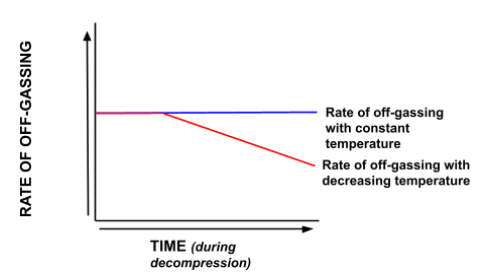
Similarly, the use of hot-water/electric heated suits at depth means that our cells will be even more vasodilated, and thus on-gassing at a higher rate than perceived by our computer/decompression algorithm. Therefore, we will have a higher amount of dissolved inert gas at the beginning and end of the decompression than calculated.
Hypothetically, being cold from the beginning to the end of the dive is less of a problem, however, as on-gassing will be reduced in the beginning of the dive anyway, so it won’t have as great an effect during the decompression. This is because there is a continuous level of vasoconstriction. However, in reality this is an unlikely situation as even if the diver begins cold, they will become much colder over the course of the dive.
Obesity

When Caisson workers began recording their symptoms and specific cases, there was a noted increase in the amount of decompression sickness cases suffered by overweight, out-of-shape workers compared to fitter workers. This trend has also been observed in modern diving.
Some researchers have suggested that it is not being overweight in and of itself that increases the risk, but that overweight divers tend to be less fit and are more likely to have other health problems, thereby increasing the risk of developing DCS. On this subject, many health consequences of obesity, such as coronary heart disease or diabetes, are contra-indications to diving themselves.
A fit individual who exercises regularly is at a much lower risk of DCS compared to an unfit diver. Regular cardiovascular exercise is believed to have a significant effect in reducing the risk of DCS. With better cardiovascular health comes better perfusion and gas exchange. Similarly, weight training strengthens the bones by increasing bone mineral density. This is believed to help prevent the onset of dysbaric osteonecrosis in divers, thereby preventing type 4 DCS.
There are at least three general reasons accounting for why obese divers are at a higher risk of decompression sickness.
1. Nitrogen is 5 times more soluble in fat than in muscle.
This leads to a far higher level of nitrogen loading in fatty tissues, and the more fatty tissues there are, the higher the nitrogen loading. This has two consequences.
Firstly, real inert gas tissue loading is going to be higher than that predicted by the dive computer/decompression algorithm, meaning a greater amount of decompression will be required than accounted for by the dive computer.
Secondly, this greater overall tissue loading poses a greater risk for repetitive diving, especially repetitive decompression diving, as the highly loaded slow tissues will have more gas for supplying bubbles with, leading to greater bubble growth.
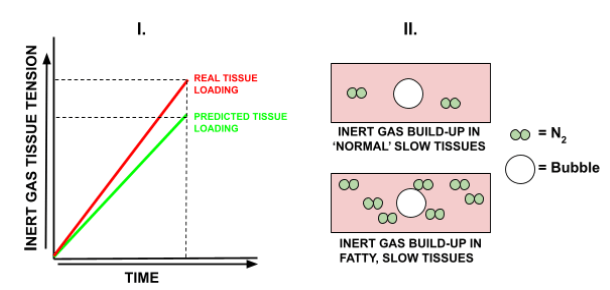
2. Fatty tissues are poorly supplied with blood vessels (poorly perfused).
This causes slowed off-gassing, which combined with the high solubility of nitrogen increases the risk of DCS, as well as exacerbating bubble growth in repetitive dives.
3. Fatty tissues have higher blood lipid levels.
Blood lipids are believed to be triggers for bubble formation.
Pre & Post-Dive Exercise

Exercise before, during and after the dive has been shown to have a significant effect on the risk of developing decompression sickness.
Exercising during the bottom portion of the dive puts the diver at increased risk. This is because with more movement and exertion there is increased blood flow, meaning a higher rate of on-gassing. The problem is that this higher rate of on-gassing is not accounted for by the decompression algorithm, thus resulting in the diver completing less decompression than actually required. Therefore, the less exertion during the bottom portion, the less on-gassing, and the lower the risk of DCS becomes.
For the decompression portion of the dive, it is not so clear with regards to exercise. It is believed that there is an optimum amount of exercise during decompression. Exercise increases blood flow and thus the rate of off-gassing. This could be simply light/medium swimming. In this case, light exercise could in fact help us to decompress better. However, excessive exertion will lead to an increased risk of bubbling and so should be avoided.
Similarly, within at least the first hour after surfacing (if not longer), exertion should be kept to the minimum, as this is the point in which there is the highest amount of bubbles present. This is sometimes referred to as the ‘final deco stop’ as it should be treated as such. Heavy lifting and/or cardiovascular exertion puts the diver at a significantly increased risk of developing DCS. This was noticed as early as with Caisson workers, who were advised to take at least one hour of rest post-surfacing.
Smoking

The respiratory system is a key player in decompression, and thus any effect on lung function will have an effect on decompression outcomes.
It is primarily the long-term consequences of smoking that increase the risk of decompression sickness, rather than the short-term effects.
Long-term damage from smoking causes Chronic Obstructive Pulmonary Disease (COPD), which is inclusive of emphysema and bronchitis. These obstructions occur in the alveoli and can result in air-filled dilations that trap gas, consequently leading to a significantly increased risk of pulmonary barotrauma and arterial gas embolism.
Bronchial mucous production is also far higher in smokers, coupled with paralysis of the cilia which serve to remove dust and unwanted particles out of the lungs. This can increase the chance of mucous plugs, which again trap gas bubbles. This leads to an increased risk of rupture upon ascent, i.e. arterial gas embolism.
Smoking, as with obesity, significantly raises the chance of having other consequential health problems, which could be contra-indications to diving, or at least affect off-gassing rates.
Carbon monoxide (CO) retention is also a big factor as it reduces the ability for oxygen to bind with haemoglobin, hindering gas transport during off-gassing. Cigarettes contain high levels of CO, and, when dissolved in the blood and then pressurised (when diving), this can increase bodily CO to extremely high levels.
Equally, nicotine acts as a vasoconstrictor, which hinders off-gassing. This is especially the case when divers smoke just after surfacing, thereby causing their blood vessels to immediately constrict, slowing inert gas washout. This is then far more dangerous if the diver is to make repetitive dives as the total amount of dissolved inert gas in the tissues will be higher than calculated by the decompression algorithm.
Age
The idea that the risk of DCS increases proportionally with age is disputable. Age alone is unlikely to increase the risk of DCS.
However, it is the by-products of aging which have the potential to increase the risk of DCS. The older a person is, the more likely they are to have health problems, be unfit and have contra-indications to diving.
There is evidence that more gas nuclei may be present in the tissues of older people, especially in the spine. However, the scope of this risk is unlikely to be significantly higher.
Dive Profile

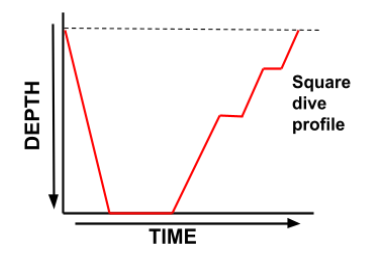
The ideal dive profile is one in which the deepest part of the dive comes earliest, followed by a gradual ascent back to the surface, in which the depth becomes continuously shallower. This is referred to as a ‘square’ profile, as demonstrated in Figure 3 below.
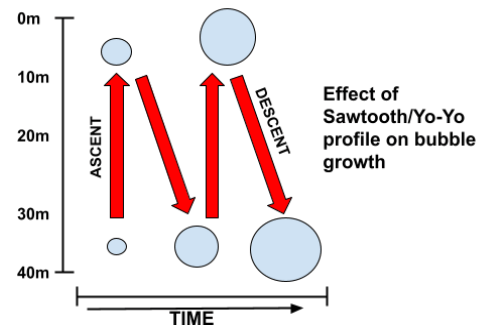
Conversely, a dive profile with continual changes in depth (known as a ‘Yo-Yo’ or ‘Sawtooth’ profile) increases the risk of decompression sickness due to bubble mechanics. This type of profile is demonstrated in Figure 4 below.
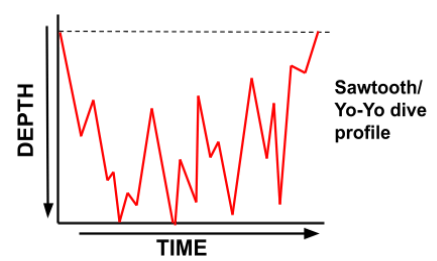
The internal pressure of a bubble is determined by the ambient pressure plus the surface tension. The bigger the bubble is, the lower the surface tension.
When a diver ascends rapidly from depth, giving the bubble insufficient time to shrink, the internal pressure will rapidly drop due to the sudden decrease in ambient pressure. The surrounding tissues may be saturated to a higher pressure than the internal bubble pressure as a result.
Consequently, gas will then rush into the bubble, out of the higher pressure tissues, causing it to grow.
Not only does this result in a larger bubble, but consequently a lower surface tension. This means that when the diver again descends the bubbles internal pressure will now be lower than it was at the same previous ambient pressure, making growth more likely.
Repeat this multiple times and the diver will have formed numerous large-sized and growing bubbles, increasing the risk of decompression sickness substantially.
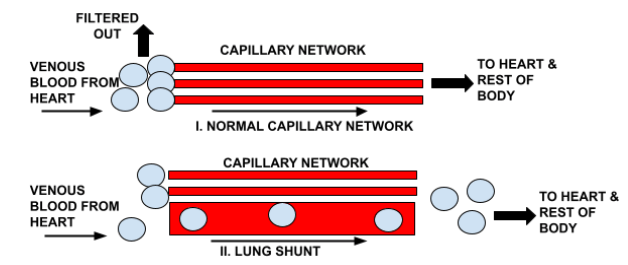
Similarly, by redescending every time, the bubbles will shrink just enough to escape past the capillary lung filter, into the arterial blood. On ascent, these will then expand and lodge in the tissues. Figure 5 below demonstrates this process of bubble growth.
Reverse Profiles

Reverse profiles refer to repetitive diving in which the next dive is deeper than the previous dive (for example, diving to 40 metres after having just dived to 20 metres).
Historically, recreational training agencies have advised against reverse profiles, claiming that they increase the risk of decompression sickness. However, this recommendation actually has no evidence to support it, and rather became lore by mere propagation.
The US Navy, recreational dive professionals, and the commercial diving industry have performed reverse profiles for decades without incidence. There is no scientific/physiological basis to argue against reverse profile.
However, from an efficiency point of view, there is an argument (NDLs, nitrogen loading).
That being said, if performing repetitive decompression dives within less than 4 hours of each other, it may even be advisable to in fact use a reverse profile. This is because a deeper profile will allow better compression and decompression of existing bubbles from the first dive.
Patent Foramen Ovale
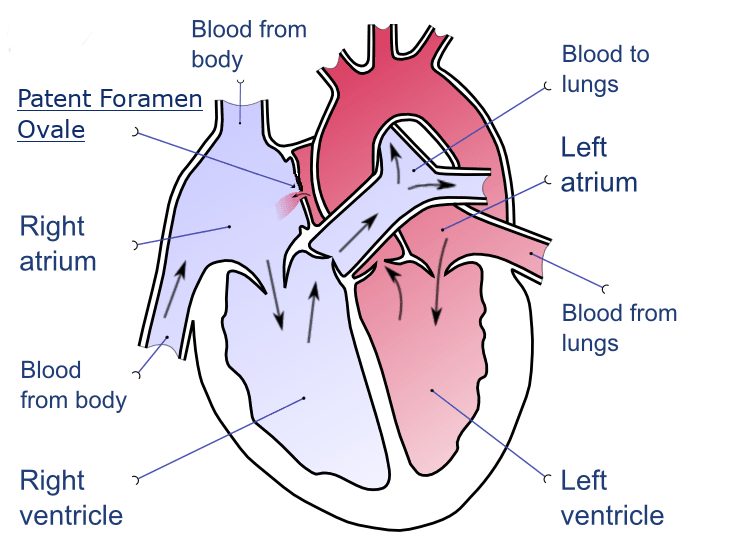
Patent foramen ovale (PFO) refers to a ‘hole’ that exists between the top chambers of the heart. This hole is something present in all fetuses but it is usually sealed upon birth. However, approximately 25% of adults still have a PFO due to it not properly sealing after birth.
A PFO will have no symptoms and will be largely harmless. However, it can prove to be a significant risk for divers.
PFO’s account for 75% of ‘undeserved DCS hits’, and are thought to be linked to skin bends, as previously mentioned (Powell, 2016).
The way in which a PFO affects a diver is that it allows blood to pass from the right atrium to the left atrium before passing through the lungs.
Normally, deoxygenated venous blood passes from the right atrium, through the right ventricle and away through the pulmonary artery to the lungs. At the lungs, apart from picking up oxygen, the venous blood will contain inert gas bubbles which the fine capillaries of the lungs will filter out before returning to the heart. Once oxygenated blood returns to the left side of the heart it is then pumped through the aorta to the rest of the body.
What the PFO does is allow a bypass in the lung filtration stage. Venous blood containing inert gas emboli will travel from the right to left atrium and will then be sent to the rest of the body’s tissues.
A PFO, however, is not necessarily a contra-indication to diving. A diver with a PFO could do thousands of dives without incident. In order for decompression sickness to result from the PFO, the venous system must contain bubbles. The occurrence of bubbles loosely, but not causally, increases with depth and decompression obligation. Therefore, for recreational, shallow dives the risk is much less for the diver with a PFO than for deep technical dives.
Similarly, although the risk of decompression sickness is increased for those with a PFO, health experts and decompression scientists believe the risk to not be significant enough to require mandatory PFO screening for all divers.
Pulmonary/Lung Shunt

Like a PFO, a lung shunt allows inert gas emboli to bypass the capillaries, resulting in them reentering the heart and being sent to the rest of the body. The effect of a lung shunt is identical to a PFO.
In the lungs, there is a network of fine capillaries which effectively act as a filtration system, removing inert gas emboli from the blood before it returns to the heart to be pumped around the body again. When a lung shunt is present, there is a larger blood vessel within the capillary network which allows the bubbles to escape the capillary filtration mechanism, thereby allowing a return to the heart. Figure 6 demonstrates this visually below.
Drugs

The effects of over-the-counter and prescription drugs are widely unknown, but are definitely not without consequences in some cases.
Any drug that can change the circulatory system or lung function can have an impact on the risk of developing decompression sickness. Similarly, any drug that affects the central nervous system has the potential to increase susceptibility to oxygen toxicity, suppress cognitive ability, and exacerbate narcosis.
For example, certain anti-malarials, decongestants, anti-histamines, and even erectile dysfunction medication all have the potential to alter inert gas uptake and washout.
The potential effects of these drugs (among the hundreds of thousands of others in circulation) in a hyperbaric environment is largely unknown, and the individual diver should research and perhaps even consult their physician or Divers Alert Network (DAN) before diving with this drug.
Previous Decompression Sickness

Divers who have previously suffered from DCS are more likely to suffer it again.
This is because DCS causes tissue damage which is often permanent. This tissue damage affects tissue perfusion as well as blood flow, which changes the on/off-gassing mechanism.
This, of course, can make DCS more probable.
Overall, it can be seen that there are many factors that contribute to our risk of developing decompression sickness. Similarly, there are likely other factors not mentioned here that we do not even yet know about. Luckily for us, however, many of these factors are controllable. Stay tuned with our Education series for more in depth, no fluff content like this this.