As divers, we face a particular set of risks unknown to the non-diving community. One of the major risks, peculiar only to diving, is decompression sickness (DCS for short). But what exactly is DCS? How does it arise? Does it vary in severity?
In this article, as part of our on-going Education series, we are going to dig deep into DCS, the physiological mechanisms behind it, as well as its history. Read along to fine tune your understanding.
History of Decompression Sickness
Decompression sickness results when inert gas dissolved in the body’s tissues comes out of solution forming bubbles. At a certain size and/or level of bubbles, nerves will be impinged causing pain, and – in more severe cases – oxygen deprivation will occur in tissues downstream of the bubbles, often leading to long-term damage.
Before delving into the science behind DCS, it is useful to look briefly at its history.
Robert Boyle (1627-91)
The first record of DCS comes from that of seventeenth-century scientist Robert Boyle (the same Boyle who gave us Boyle’s Law). He first observed the phenomenon of DCS when studying the effect of different pressures on animals. While decompressing a snake inside a vacuum (i.e. reducing the ambient pressure), Boyle noticed that the snake was ‘furiously tortured’ and, on closer inspection, observed a small bubble ‘moving to and fro’ in its eye (Powell, 2016). This was the first recorded instance of DCS, although its cause was not yet understood.
Caisson’s Disease
More than two hundred years later, at the beginning of the nineteenth century, DCS was again observed. This time, however, in humans.
In the midst of the Industrial Revolution, underwater construction work was on the rise. An innovation during this time was the ‘Caisson,’ which was a type of dry diving bell that allowed workers to undertake long projects in pressurised environments. However, over time, Caisson workers complained of symptoms such as joint pain, breathing difficulties and dizziness, after having returned to surface pressure. Similarly, they noticed that the symptoms dissipated when re-pressurised in the Caisson. This became known as ‘maladie du caisson,’ i.e. Caisson’s disease.
As the use of Caissons continued, it was observed that the frequency and severity of symptoms got worse with increased pressure as well as time spent at the given pressure. Many Caisson workers were permanently paralysed and some died too.
Similarly, it was also noted that symptoms were not as severe or frequent when the workers were depressurised slowly.
When the Brooklyn Bridge was constructed over the period between 1870-83, the rate of Caisson’s disease was very high. So high, in fact, that the disease was renamed. Caisson workers, suffering from joint and abdomen pains, frequently struggled to stand up straight, and their posture was compared to that of the fashionable ‘Grecian bend’ of the time. Thus, Caisson’s disease was renamed ‘the bends’ (Powell, 2016).
Paul Bert (1833-86)
In the same century, French scientist Paul Bert made groundbreaking discoveries in the field of hyperbaric science. In one experiment, Bert compressed 24 dogs to a pressure of approximately 87.5 metres and then decompressed them back to surface pressure within four minutes. 21 of the 24 dogs died. He repeated the experiment, this time, however, decompressing the dogs over the course of more than one hour. In this case, all of the dogs lived and none suffered any symptoms of DCS (Powell, 2016).
Bert observed that it was the high partial pressure of nitrogen that caused the problems, dissolving in the body’s tissues and coming out of solution to form bubbles. Consequently, he advised that Caisson workers decompress gradually and at a constant rate.
Similarly, he also observed that a return to pressure, i.e. recompression, could alleviate the symptoms of Caisson’s disease, and that supplementing this with the breathing of oxygen accelerated the process of recovery.
Thus, Bert not only discovered the origin of DCS; he discovered the cure too.
John Scott Haldane (1860-1936)
Scottish scientist John Scott Haldane is most famous for his work with the Royal Navy Deep Diving Committee. Over the course of his research and experiments, Haldane concluded that gas is absorbed and released by the tissues at differing rates, and that there is a safe maximum limit to the degree to which tissues can become supersaturated without forming bubbles (causing DCS). Thus, Haldane was the first to apply the concept of half-times to diving physiology as well as laid the scientific basis for M-Values.
Robert Workman
Robert Workman, a scientist with the US Navy Experimental Diving Unit (NEDU), built upon the work of Haldane. Workman proposed the concept of M-Values. Similarly, in contrast with Haldane’s theory that tissue tension could not safely exceed twice the ambient pressure, Workman produced a decompression model that had multiple tissue compartments with differing half-times.
Decompression Sickness: The Chain of Events
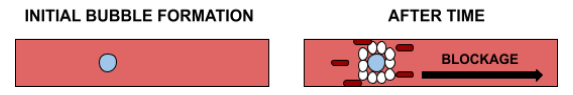
DCS is caused by the formation of bubbles in the bloodstream. Bubbles form when tissues are supersaturated to too high a degree.
During supersaturation, dissolved inert gas (in solution) moves out of the tissues and into the bloodstream. This occurs on the ascent portion of every dive, hence the popular phrase ‘every dive is a decompression dive.’ Thus, supersaturation is not inherently bad, but is in fact necessary to every dive.
However, if the pressure difference between the dissolved gas in the tissues and that of the ambient pressure is too great, gas will not be able to leave the tissue at a quick enough rate while remaining in solution. Thus, the gas will be forced out of solution in bubble form. This is known as ‘critical supersaturation.’ These bubbles get caught in all parts of our body, causing an array of problems. The point at which the pressure difference becomes too great is when the pressure difference is in excess of the M-Value of a given tissue.
The Chain of the Bubble
An inert gas bubble can cause nerve and tissue damage due to impingement and blockage. The latter can result in oxygen starvation and thus permanent tissue damage.
However, it is not the work of the inert gas bubble alone which causes the symptoms of DCS. It is the combined work of the bubble and the body’s immune system response.
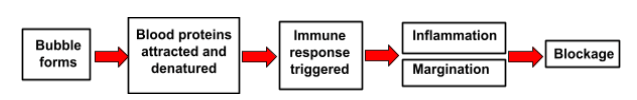
An inert gas bubble attracts blood proteins, which upon contact with the bubble will be denatured. This triggers the body’s immune response, as the denatured blood proteins are now deemed to be a foreign body.
Part of this immune response is the release of histamines by the mast cells, which causes inflammation, as well as the process of ‘margination’ in which the blood vessel walls become sticky in order for the white blood cells to surround the foreign body and then stick to the walls in a clump form. This, of course, causes blockage.
Margination also results in the separation of the endothelial cells (those in the walls of the blood vessel), allowing more fluid and white blood cells to flow through. This separation is treated as an injury site by the body, and so platelets are sent to the area, which combine with collagen to clot. This clotting further reduces blood flow, blockage, and inflammation.
This is the basic physiological mechanism behind Type 1 & 2 decompression sickness.
This chain of events takes time to develop, hence why DCS is not usually experienced immediately upon surfacing. It requires not only the presence of bubbles, but the triggering of the body’s immune response to those bubbles, before becoming symptomatic.
The quicker one is recompressed, the sooner this chain can be stopped from developing and permanent damage prevented.
Symptoms
Although the symptoms of DCS can vary from person to person, the most common ones are as follows.
- Joint pain – joint pain is by far the most symptom of DCS, particularly in the upper body, such as the shoulders.
- Arm pain or sensation
- Leg pain or sensation
- Dizziness
- Paralysis
- Shortness of breath
- Extreme fatigue
- Unconsciousness
Similarly, in accordance with the US Navy Diving Manual, the time of onset of symptoms (after surfacing) is estimated as follows (Powell, 2016).
- Within 30 minutes = 50 % of cases
- Within 60 minutes = 85 % of cases
- Within 3 hours = 95% of cases
Delays in excess of 3 hours are usually due to the diver not noticing the symptoms as opposed to an actual delay in the appearance of the symptoms.
Classifying the Bends
Type 1 Decompression Sickness
Type 1 DCS is typically considered as a ‘minor’ or ‘pain only’ bend, usually resulting in joint pain, a rash and/or itching of the skin.
Type 1 cases often resolve without formal treatment, however, observation by a specialist is always recommended as ‘minor bends’ can be a precursor to more serious forms of DCS. Similarly, in all cases, the breathing of oxygen will help massively in the alleviation of symptoms.
Pain-Only Bend
Accounting for the overwhelming majority of cases of DCS, joint pain is the most common symptom.
It is most commonly described as a throb or deep ache. For recreational divers, this is most often in the upper body joints, such as the shoulders and elbows.
The cause of the pain is actually still unknown and is not caused by the formation of bubbles alone.
Although very common, joint pain remains one of the most treatable symptoms of DCS, with patients’ pain often being alleviated before the chamber is fully pressurised to its target depth.
Skin Conditions
Skin conditions are also a common manifestation of type 1 DCS. They can be anywhere from mild to very serious. Generally, there are three conditions: Pruritus (itching), Cutis Marmorata (skin marbling), & Localised Pitting Edema.
Pruritus (itching)
The most benign of skin conditions is pruritus (itching). Often, there are no visual changes in the skin and the itching is transient and mild, mostly occurring around the ears, hands and wrists.
This form of DCS does not normally require recompression, and will resolve itself without treatment – but, of course, the breathing of oxygen will significantly aid this process and is advised.
What is noteworthy with pruritus, however, is that if a diver suffers it on multiple occasions, it may be a sign of a PFO (patent foramen ovale), and, therefore, those who suffer regular occurrences of pruritus should be screened for a PFO.
Cutis Marmorata (skin marbling)
Those suffering from cutis marmorata (skin marbling) should seek an assessment from a specialist, as it is often a precursor to far more serious types of DCS, i.e. type 2 DCS.
Skin marbling usually occurs as a violaceous mottling on the torso, and is extremely itchy due to a localised subcutaneous vascular reaction from the bubbles. It is sometimes preceded by full torso itching and a burning sensation.
The breathing of oxygen, specialist examination and recompression are all necessary.
Localised Pitting Edema
Localised pitting edema is again indicative of a more serious type of DCS to come.
It is characterised by a pitting of the skin (in which the pressing of the skin’s surface leaves an indentation) that is called peau d’orange, which translates to ‘skin of an orange’. This manifests over the torso.
Edema simply refers to the swelling of the skin due to a buildup of fluid, caused by the bubbles blocking the dermal and subcuticular lymphatics.
The breathing of oxygen, specialist examination and recompression are all necessary, with victims requiring immediate medical attention.
Type 2 Decompression Sickness
Type 2 DCS is far more serious and life-threatening, often leaving the victim with long-term or even permanent damage. It has two primary categorisations:
- Neurological Type 2 DCS.
- Cardiovascular/pulmonary Type 2 DCS.
Neurological DCS
The term ‘neurological’ refers to that which affects the nervous system. Thus, neurological DCS occurs when bubbles are transported into the nervous system.
The presence of bubbles in the nervous system will disrupt transmission mechanisms, resulting in numbness or paralysis. If bubbles affect transmissions in the brain or spinal cord, the following can happen:
- Visual disturbances
- Loss of bladder or bowel control
- Hearing loss
- Cognitive impairment
- Loss of balance and coordination.
Similarly, lower back pain and/or pain encircling the abdomen is symptomatic of a spinal decompression problem.
Memory, reasoning and speech may also be affected in both the immediate short-term and long-term. This is known as ‘cerebral bends.’ Consequently, it is necessary for others to assess the state of the victim in order to gauge the severity of their condition.
Cardiovascular/Pulmonary DCS
Cardiovascular/Pulmonary DCS occurs when bubbles accumulate in the lung capillaries that surround the alveoli. This can occur at low levels of bubbling without incident.
However, at a certain level, the bubbles accumulate and begin to decrease lung efficiency. This results in a dry, persistent cough and develops into serious breathing difficulties. This type of DCS is nicknamed ‘the chokes,’ given the consequent impairment to breathing.
Type 3 Decompression Sickness
Unlike type 1 and 2 DCS, type 3 and 4 are largely unknown, even among recreational divers. There is a good reason for this.
Type 3 DCS is exclusive to technical divers using trimix below 100 metres, while type 4 DCS is a long-term condition, still largely unknown about.
Type 3 DCS is also known as Vestibular or Inner Ear DCS.
Inner Ear DCS is a very rare form of decompression sickness as it affects only those diving with two inert gases at play (i.e. helium and nitrogen), and usually only at depths equal to or greater than 100 metres.
It is closely related to the concept of Isobaric Counter Diffusion.
Simply speaking, the inner ear is composed of three compartments with varying levels of perfusion. When switching from a helium rich mixture to a nitrogen rich mixture, the nitrogen diffuses into the tissue of one part of the inner ear at a rate quicker than the helium leaves the other part. This causes overall inert gas tissue tension to rise, resulting in DCS.
Symptoms of type 3 DCS are severe vertigo, nausea, hearing loss and dizziness.
Type 4 Decompression Sickness
Probably the least common of classifications, type 4 decompression sickness refers to the long term condition of dysbaric osteonecrosis (DON).
Simply, this is bone cell death as a consequence of exposure to fluctuating pressure.
This is believed to be caused by bubbles blocking blood vessels within bones during decompression, resulting in cellular death and/or bone cancer, along with an array of other bone related problems.
DON is a condition, it seems, that can affect almost all divers. The risk does seem to increase with depth, duration and exposure, but these are not necessarily the causal factors. It seems that it may have more to do with the ‘quality’ of decompression rather than purely depth alone.
Conclusion
Now that we have established the cause of decompression sickness and its various classifications, be sure to check out the next article in our Education series: Decompression Sickness: Predisposing Factors.
References
(1) Powell, Mark (2016) Deco for Divers: A Diver’s Guide to Decompression Theory and Physiology, United Kingdom: Aquapress Limited.